There is little awareness amongst the public about the dire circumstances of older adults and seniors living homeless because of mental health challenges. Oregon law sets a high bar for hospitalizing adults who are unable to consent to care which can leave them living in inhumane and dangerous conditions. Peer support specialist, Duke Reiss, explains what it looks like to try to find help for a senior with high-level needs with no income or family to rely on.
By Duke Reiss
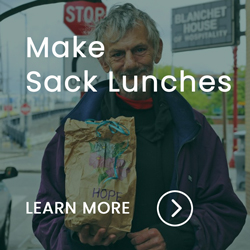
I have been a peer support specialist in Portland, OR, since 2021. Before that, I worked primarily with people who were experiencing homelessness. First, as a case manager and then as a staffer in a shelter. In my current role at Blanchet House, I support members of the public who are struggling with many challenges like addiction, mental health, and other disabilities. Peer support specialists like me view our clients as equals, so we refer to them as “peers” instead of clients.
I am often asked what the hardest aspect of my work is. What comes to mind immediately, is witnessing seniors (people aged 60 or higher,) in our community who are unable to access needed services. I see seniors forgotten about. For example, if a senior has acute symptoms of mental or physical health needs, they can be blacklisted from shelters. The reason is that they cannot take care of themselves like bathing or eating, so they are denied services. Their needs are too high for shelter staff to address.
This is such a prevalent problem in our community. Most emergency shelters ask potential clients during the intake process if the individual can care for themselves. This is because many people on the streets should be in assisted living or supportive housing facilities with 24-hour caregivers. Homeless shelters are not adult care facilities.
My job intersects with these high-needs seniors when they come to Blanchet House to access food. I get to know them and work to get them into assisted living. However, these same seniors denied a bed at shelters are also told that they don’t qualify for assisted living. The reasons can range from they are too capable of caring for themselves or that there is no space available.
There are also many red-tape barriers to getting a senior off the streets and into assisted living. A potential candidate will need identification, an income like social security, sobriety, and many assessments to determine if they meet the qualifications of the facility. All these processes combined take months to complete but trying to do them all while living in terrible conditions on the street can take years to address. Especially with people unable to stay in one location.
In addition, these vulnerable adults often bounce between multiple case managers, which starts the laborious process over. Giving consent is the first step to this long grueling process of getting into assisted living. I work with many seniors who are open to assisted living but have acute cognitive challenges such as schizophrenia or head trauma that make it hard for them to understand and consent to the process. These seniors often are unable to even sign their names or partake in an assessment.
What happens when older adults with acute mental health needs are unable to consent to care in Oregon?
They often end up houseless on the streets, using low-barrier nonprofits such as Blanchet House to meet their basic human needs for survival. Low-barrier service providers don’t require their name which can be lifesaving since some people are incapable of even verbally providing their name. Untreated mental health is a constant obstacle to being able to consent to services that could end a person’s suffering and homelessness.
In this situation, outreach workers like me can’t help, nor can any shelter. Even the county’s Adult Protective Services (APS) and Aging and Disability Services (ADS) can only do so much if someone cannot consent.
Well, what about self-neglect cases?
In theory, if someone is a danger to themselves or others a self-neglect case can sometimes be opened.
I have been told by APS and ADS that behavioral health neglect is a lot harder to investigate than physical neglect. Behavioral health neglect cannot be investigated until the individual reaches the age of 65, while physical neglect can start being investigated at the age of 60. If someone cannot consent, getting care can be impossible even for people living in inhuman conditions on the streets. I’m referring to people aka peers who are defecating on themselves, not eating, unable to hold a conversation, and/or getting into fights they won’t recall in an hour. These same seniors will be begging to get off the streets, but they don’t have the capacity to understand that they need to sign paperwork to give consent.
Sometimes people experiencing severe mental health issues can scare county workers away because they may yell or seem threatening. It can be difficult to know if they are yelling at you or an unseeable fear of theirs. Often, they are recounting their trauma. But in a context that makes others feel like they are being insulted or threatened because it is hard to follow what they say.
An Involuntary Commitment Program (ICP), is an involuntary hold of an individual done at a hospital. It is sometimes an individual’s only hope for getting help. This hold can allow the individual time to get back on their medications, and be in a more stable environment with a roof over their head. The problem is, that once a person is there for three days, they are denied the ICP program. This is because they are often deemed stabilized when they have not yet reached their baseline.
When can APS and ADS get involved in ICP?
For some people who cannot consent to care, receiving an ICP hold is their only shot at getting back on their medications. For better, or for worse, ICP criteria to receive an involuntary hold can be very strict and specific.
Recently, I was informed by APS and ADS that a peer (aka client) of mine, who has been unable to consent to services since before 2018, could now possibly receive help because she turned 60 years old. However, she could not receive help because of her mental health diagnosis. Instead, they had to ignore the diagnosis and focus on her physical decline. They could only focus on her mental health diagnosis after she turned 65. Any effort to pursue a self-neglect case based on this peer’s mental health diagnosis may face denial until she reaches the age of 65. This can be disastrous for someone whose main barrier is coping with mental health such as a diagnosis like schizophrenia or bipolar.
A person who is unable to consent to shelter or outreach has fallen between the cracks of care. For my peer, only now that she’s 60 years old, is there any hope of getting her the help she deserves. But even then, it has been months since she turned a qualifying age. It will continue to be a long strenuous process that she may not survive the winter to see.
What can be done?
It starts with state and county laws. Laws that contain too specific criteria make it impossible for qualified social workers to advocate for a peer. The peer must be able to go in front of a judge to have the county take custody of them. Under current law, county and social workers must work loopholes to try to get someone the care they need. These laws save the county and state money. But for peer support specialists to save lives we need the ability to advocate for the care of our clients.
You can read more about one woman’s challenges to receiving care in Portland as reported by Nicole Hayden in The Oregonian here.
Acknowledging the trauma and discrimination of civil commitment
I want to finish by acknowledging the trauma and discrimination often endured when in a civil commitment or any kind of hold. I only experienced a taste of the fear, stress, and re-traumatization that can happen in a hold, especially for minorities based on race, gender, ability status, and sexuality. I do believe there is a time when a hold is the only option available. I know this to be true for myself, and for everyone who has the potential to be harmful to themselves or others. Holds should be utilized only when critically necessary. It should still be easier for qualified professionals to submit for a hold evaluation, so more people can access the situation, thus not relying on one possibly biased perspective. But holds should never be done flippantly and without careful consideration if there are other resources, such as advice from peer support or recovery mentor, follow-up appointments for medication, and follow-up procedures to ensure they have access to ongoing therapy.